Treatment
Antibiotics and Synthetic TB Drugs
The first antibiotic found to be effective against tuberculosis was discovered in the lab of Selman Waksman in 1943. Streptomycin, developed from soil fungus, killed tuberculosis bacteria but had some severe side-effects, including dizziness, fever, headache, nausea, loss of balance, and/or deafness. It was also soon found that TB bacteria were able to develop resistance to streptomycin. As a result, streptomycin and para-amino salicylic acid (PAS), a synthetic drug also discovered in 1944, were jointly prescribed, limiting the development of drug resistant bacteria.
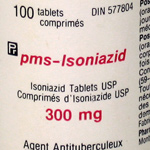
Isonicotonic hydrazide, most commonly called isoniazid, was found to be effective against tuberculosis in 1952. Though having fewer side-effects than streptomycin, when prescribed on its own isoniazid also created drug resistant strains of TB. When prescribed with streptomycin and PAS the incidence of drug resistance decreased. This cocktail of drugs was the first to cure tuberculosis and formed the basis of TB treatment in Canada until the 1970s.
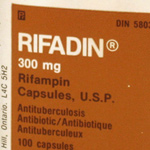
Today, tuberculosis is typically treated with a six-to-twelve month course of isoniazid, rifampin, and pyrazinamide or ethambutol.
Side effects to this drug regimen can be quite severe. Rashes, itch, fever, dizziness, nausea, fatigue, joint pain, and liver failure are but a few of the possible effects. As a result, some patients discontinue their treatment plan rather than experience these side-effects. In turn, stopping treatment early creates drug-resistant strains of the bacteria. Part of the World Health Organization’s Directly Observed Therapy Short-course (DOTS) program involves greater supervision of treatment in an attempt to stop treatment drop-out and the development of drug resistance.
Explore the picture gallery to learn more about this treatment.