A Brief History of Isolation and Infectious Disease
Drawing about the Cholera in Le Petit Journal, c. 1912
Contagious disease has challenged society throughout human history. Quarantine and isolation was practiced in response to the pandemics of bubonic plague and cholera, beginning in the Middle Ages. In the 18th and 19th centuries, smallpox led to smallpox hospitals in some large urban communities. At the same time, citizens lived with the fear of outbreaks of typhus, typhoid fever, diphtheria, scarlet fever and influenza. The effectiveness of isolation was often limited due to the lack of knowledge of the cause and transmission of these infectious diseases.
The germ theory of infectious disease was formulated during the second half of the 19th century. In the absence of specific treatment, isolation became the principle strategy to prevent the transmission of contagious disease. The Ontario Public Health Act in 1884 provided for the expropriation of land for isolation hospitals and required separate facilities for smallpox. Kingston established a Board of Health and created high standards of quarantine with a freestanding isolation hospital and the isolation of contagious disease in the home.
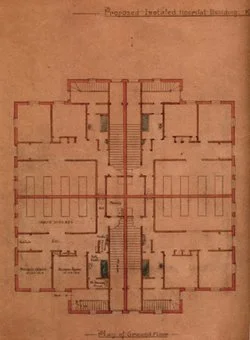
The Nickle Wing of the Kingston General Hospital, one of the earliest isolation facilities in Canada, served the community from 1892 until 1922. The chair of the Board of Health found the structural precautions to isolate this wing from the main building good but not as efficient as where contagious cases are cared for in separate buildings. This was achieved with the opening of the freestanding isolation hospital in 1923.
The Board of Health required quarantine with isolation in the home by 1899. Whenever a case of smallpox, cholera, scarletina, diphtheria, whooping cough, measles, mumps, or other contagious diseases existed in any household belonging to which were persons attending school, no member of such household was to attend school until a certificate had been obtained that infection no longer existed in the house.
The introduction of public health defenses included improved sanitation and safe water to prevent cholera and typhoid fever; vaccines that lowered the incidence of smallpox, diphtheria, pertussis, tetanus, rubella, measles, mumps and polio; and the discovery of antibiotics to treat specific infectious disease. Extrapolating from these dramatic advances, many concluded that infectious disease could be prevented or easily managed. During the 20th century, the practice of isolation in hospital and the home declined.
H1N1 Warning Notice, Image: Kingstonist.com
In recent years, even developed countries have discovered that they remain painfully vulnerable to infectious disease. The reemergence of antibiotic resistant organisms such as staph aureus, c. difficile, and tuberculosis particularly in the immune deficient contribute to nosocomial infections in hospitals, nursing homes and the community, while epidemics of cholera occur due to failure of sanitary conditions. The emergence of mutations of the influenza virus leading to pandemics such as the SARS outbreak for which there is little or no specific treatment are annual concerns.
These infections again require isolation in hospital and the community. The lessons learned in the 19th century are particularly relevant to these present day challenges.
James Low, Executive Director
A version of this blog post is also available as an hour-long video presentation.