Diagnosing Tuberculosis
There are a number of diagnostic tests used to find out whether a person has been infected with tuberculosis at some point, meaning they may have a latent case of the disease or may have cured themselves, or whether they currently have the active disease. The nature of tuberculosis, its ability to lay dormant within the body for years, means that determining that a person has been infected with tuberculosis is not enough to know whether they are presently capable of transmitting the disease. Multiple types of tests are often required to accurately diagnose cases of tuberculosis.
Past exposure to tuberculosis, and the current possibility of either latent or active TB, is indicated by skin and blood tests that measure the body's immune response to TB antigens. These tests indicate only that an individual has once had the TB bacteria in their system, not whether the disease is still present. They are useful insofar as a negative result is a fairly accurate indicator that the individual does not have TB. A positive result requires further diagnosis to conclusively identify whether it is a case of active or latent TB.
Active tuberculosis is suggested by presentation of the signs and symptoms of TB, as well as by tests that seek to find tuberculosis bacteria in sputum. Though such tests have taken weeks to conduct in the past, making them an imperfect diagnostic tool, new technologies have made the process of identifying Mycobacterium tuberculosis move much more quickly.
Click on any of the following diagnostic methods to open a picture gallery and learn more about how the test works.
Testing for Latent Infection
-
 A skin test is most commonly used to test for tuberculosis. A small amount, 0.1mL, of purified protein derivative (PPD) tuberculin is injected intradermally, under the skin of the forearm.
A skin test is most commonly used to test for tuberculosis. A small amount, 0.1mL, of purified protein derivative (PPD) tuberculin is injected intradermally, under the skin of the forearm.
Injecting tuberculin as part of the Mantoux Tuberculin Skin Test.
CDC PHIL #6806, CDC/Gabrielle Benenson -
 Within 48-72 hours of the injection, the site will be examined for reactions, such as swelling, hardness, and blistering by a health care professional. They will measure the induration (raised area) and compare the measurement to standards, and patient history, to ascertain whether the reaction is a positive indication of infection.
Within 48-72 hours of the injection, the site will be examined for reactions, such as swelling, hardness, and blistering by a health care professional. They will measure the induration (raised area) and compare the measurement to standards, and patient history, to ascertain whether the reaction is a positive indication of infection.
Positive TB skin test result
© Wellcome Trust -
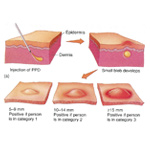 For example, the American Center for Disease Control and Prevention notes that an induration of 5 millimeters is considered positive for persons with HIV, who have had organ transplant, or who have been in recent contact with an infected individual, while an induration of 10 millimeters is required for a positive result for recent immigrants, injection drug users, children under 4 years of age, and some lab personnel. For people with no known risk factors for TB an induration of 15 millimeters would be considered a positive result; however, such individuals would rarely be given a skin test.
For example, the American Center for Disease Control and Prevention notes that an induration of 5 millimeters is considered positive for persons with HIV, who have had organ transplant, or who have been in recent contact with an infected individual, while an induration of 10 millimeters is required for a positive result for recent immigrants, injection drug users, children under 4 years of age, and some lab personnel. For people with no known risk factors for TB an induration of 15 millimeters would be considered a positive result; however, such individuals would rarely be given a skin test.
Mantoux skin text reading.
Cowan, M. K. and K. P. Talaro, Microbiology: A Systems Approach, 2d ed. (New York: McGraw-Hill, 2008). © McGraw-Hill Companies, Inc. -
 If the body has been exposed to the tuberculosis bacteria it will likely react to this injection; however, the test only indicates that the individual has been exposed to tuberculosis, not whether they have the active disease or a latent infection. If the body does not react to the injection it is likely that TB infection is not present. Even if the test result is negative, more tests may be required if signs of tuberculosis are present (e.g. coughing, chest pain, fever). Similarly, some people may have false-positive results, in particular individuals who have been vaccinated by the BCG vaccine.
If the body has been exposed to the tuberculosis bacteria it will likely react to this injection; however, the test only indicates that the individual has been exposed to tuberculosis, not whether they have the active disease or a latent infection. If the body does not react to the injection it is likely that TB infection is not present. Even if the test result is negative, more tests may be required if signs of tuberculosis are present (e.g. coughing, chest pain, fever). Similarly, some people may have false-positive results, in particular individuals who have been vaccinated by the BCG vaccine.
Positive Skin Test result.
CDC PHIL 3752 CDC/Donald Kopanoff
-
 TB blood tests, also called interferon-gamma release assays, measure the immune response to TB bacteria to assess whether infection or latent disease are likely. In this way these tests are similar to the skin tests.
TB blood tests, also called interferon-gamma release assays, measure the immune response to TB bacteria to assess whether infection or latent disease are likely. In this way these tests are similar to the skin tests.
Blood Sample
© Ocean/Corbis, 42-15559904 -
 A sample of whole blood is taken and sent to a laboratory, where it is exposed to antigens derived from Mycobacterium tuberculosis. White blood cells that recognize these antigens because of prior exposure to the bacteria will release interferon-gamma as part of their immune response (see Etiology – How it Works). The blood test measures the amount of interferon-gamma produced to assess whether the individual had been exposed to tuberculosis in the past.
A sample of whole blood is taken and sent to a laboratory, where it is exposed to antigens derived from Mycobacterium tuberculosis. White blood cells that recognize these antigens because of prior exposure to the bacteria will release interferon-gamma as part of their immune response (see Etiology – How it Works). The blood test measures the amount of interferon-gamma produced to assess whether the individual had been exposed to tuberculosis in the past.
Test results suggest the likelihood of infection only; diagnosis should also consider other test results and patient history. Blood tests provide more accurate results for individuals who have been vaccinated with BCG than do skin tests.Blood Sample in Laboratory
© Nicole Hill/Rubberball/Corbis, 42-24229323
Testing for Active Disease
-
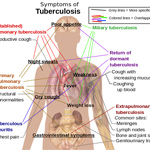 As is typically the case, one of the first diagnostic tools used by physicians to test for tuberculosis is patient history and an assessment of the signs and symptoms exhibited by the patient. The physician will review patient charts and speak with the patient about past activities, such as travel, lab work, or exposure to another infected person. They will also seek to find out whether the patient has been experiencing any of the typical signs of the disease, such as coughing, fever, night sweats, or paleness, or symptoms of the disease, such as weakness and chest pain. If these signs or symptoms are present, further testing for infection will be undertaken.
As is typically the case, one of the first diagnostic tools used by physicians to test for tuberculosis is patient history and an assessment of the signs and symptoms exhibited by the patient. The physician will review patient charts and speak with the patient about past activities, such as travel, lab work, or exposure to another infected person. They will also seek to find out whether the patient has been experiencing any of the typical signs of the disease, such as coughing, fever, night sweats, or paleness, or symptoms of the disease, such as weakness and chest pain. If these signs or symptoms are present, further testing for infection will be undertaken.
Symptoms of Tuberculosis
Image in Public Domain.
-
 Chest x-rays have been used since the early twentieth century to diagnose cases of pulmonary tuberculosis.
Chest x-rays have been used since the early twentieth century to diagnose cases of pulmonary tuberculosis.
A woman has a photofluorograph of her lungs taken.
Originally published in the Valley Echo 1943 (8): 26. Reproduced with permission of the Lung Association of Saskatchewan. -
 Chest x-rays can show evidence of active tuberculosis, or scarring and calcifications that suggest that the bacteria have been contained by the body.
Chest x-rays can show evidence of active tuberculosis, or scarring and calcifications that suggest that the bacteria have been contained by the body.
X-ray of an advanced infection of tuberculosis.
Originally published in the Valley Echo 1964 (12): 15. Reproduced with permission of the Lung Association of Saskatchewan. -
 Further tests are needed to ascertain whether the disease is currently active or latent.
Further tests are needed to ascertain whether the disease is currently active or latent.
Chest x-ray showing miliary tuberculosis.
© Wellcome Images
-
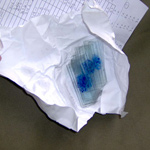 Examination of sputum under a microscope can show the presence of bacteria. This method of testing for tuberculosis has been used since the 1880s. Mycobacterium tuberculosis are acid-fast bacteria, meaning that they will stain positive with special dyes. A sample of sputum secreted from the lungs can be applied to a slide and tested for the presence of acid-fast bacilli. Not all acid-fast bacilli are tuberculosis though, so a culture of the bacteria is necessary to confirm the diagnosis.
Examination of sputum under a microscope can show the presence of bacteria. This method of testing for tuberculosis has been used since the 1880s. Mycobacterium tuberculosis are acid-fast bacteria, meaning that they will stain positive with special dyes. A sample of sputum secreted from the lungs can be applied to a slide and tested for the presence of acid-fast bacilli. Not all acid-fast bacilli are tuberculosis though, so a culture of the bacteria is necessary to confirm the diagnosis.
Sputum slides
Credit: Grace Eckoff, www.utexas.edu/features/2009/04/06/tuberculosis -
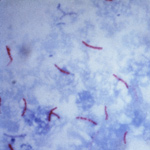 The slide will be examined under a microscope for the presence of bacteria. Here, the tuberculosis bacteria are red. Their presence indicates active infection.
The slide will be examined under a microscope for the presence of bacteria. Here, the tuberculosis bacteria are red. Their presence indicates active infection.
Mycobacterium tuberculosis, Ziehl-Neelsen stain.
CDC-PHIL ID#5789, CDC/Dr. George Kubica
-
 In addition to viewing sputum samples under the microscope, such samples are usually also cultured, meaning allowed to grow in special incubators and mediums. This method of diagnosing tuberculosis has been used since Koch’s discovery in the early 1880s.
In addition to viewing sputum samples under the microscope, such samples are usually also cultured, meaning allowed to grow in special incubators and mediums. This method of diagnosing tuberculosis has been used since Koch’s discovery in the early 1880s.
Photomicrograph of a sputum sample containing Mycobacterium tuberculosis.
CDC-PHIL #2128 -
 The growth of bacteria colonies allows lab technicians and physicians to identify the type of bacteria that is present and make a positive identification of Mycobacterium tuberculosis. These colonies are also able to be tested for drug resistance, which helps facilitate the development of treatment plans for the patient.
The growth of bacteria colonies allows lab technicians and physicians to identify the type of bacteria that is present and make a positive identification of Mycobacterium tuberculosis. These colonies are also able to be tested for drug resistance, which helps facilitate the development of treatment plans for the patient.
The bacteria replicate very slowly, though, only once every twenty four hours, and take up to one month to form a colony. Because of this, new diagnostic tools that can identify the presence of the bacteria more quickly have been sought.Tuberculosis culture.
CDC PHIL #4428, CDC/Dr. George Kubica
-
 More recent advances in tuberculosis diagnostics have focused on the detection of nucleic acids, RNA and DNA, specific to M. tuberculosis within sputum samples. Such samples can be amplified using polymerase chain reaction (PCR) to facilitate their identification, and studied to detect also gene mutations that indicate drug resistance. The advantage of this type of testing is that it takes only 24-48 hours to obtain results, as compared to cultures, which can take several weeks.
More recent advances in tuberculosis diagnostics have focused on the detection of nucleic acids, RNA and DNA, specific to M. tuberculosis within sputum samples. Such samples can be amplified using polymerase chain reaction (PCR) to facilitate their identification, and studied to detect also gene mutations that indicate drug resistance. The advantage of this type of testing is that it takes only 24-48 hours to obtain results, as compared to cultures, which can take several weeks.
Assay Procedure for MTB Test From The New England Journal of Medicine, C. C. Boehme, P. Nabeta, D. Hillemann et al., “Rapid Molecular Detection of Tuberculosis and Rifampin Resistance,” 363 n.11 Copyright © 2010 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society

